Do I Have Rosacea? What Is Rosacea? Everything You Need To Know
Including information on rosacea subtypes, causes, and 'cures'
What Is Rosacea?
Rosacea is a chronic skin condition with irregular facial flushing that can become more permanent over time. It can be accompanied by visible blood vessels, pustules, swelling, inflamed and irritated eyes, dry patches and – in severe cases – thickening of the skin.
It’s pronounced roe-zay-shuh.
What Causes Rosacea? Who Gets It?
There are many theories about what causes rosacea: genetics, bacteria on the skin, microscopic mites, inflammation, immune system issues, weaker capillaries. There are also theories about a link to the gut, hormones, trauma… the list goes on!
If someone tries to tell you that one single thing causes rosacea (usually when they’re trying to sell you something…!) they are speaking anecdotally and not scientifically.
It’s believed to be more common in women, people over 30, and people who are white with light-coloured eyes, but it can affect anyone. I wrote about how rosacea is underdiagnosed in people of colour HERE.
Are There Different Types Of Rosacea?
Yes there are a few different types of rosacea. Since 2002, we have categorised rosacea into 4 subtypes:
Subtype 1 (erythematotelangiectatic) – redness, visible broken veins, and flushing.
Subtype 2 (papulopustular) – redness and fluid-filled pimple and itchy bumps (sometimes unhelpfully known as acne rosacea).
Subtype 3 (rhinophyma/phymatous) Causes a thickening of the skin, usually on the nose. Read more about rhinophyma HERE.
Subtype 4 (ocular rosacea) This is characterised by red and sore eyes that often feel gritty. Read more about ocular rosacea HERE.
Since 2011, experts have also added another subtype to that list:
Subtype 5 (neurogenic rosacea) This is often mistaken for subtype 1, as it’s characterised by intense facial redness, often localised to the outer edges of the face. It is accompanied by debilitating pain (burning and stinging) and is resistant to the usual rosacea treatments. You can read more about it HERE.
There’s a prevalent myth that rosacea subtypes are numbered because they represent stages, e.g. you start at subtype 1 and as your rosacea progresses you then get type 2, type 3 etc. This is not true. The rosacea subtypes are standalone symptoms and categories and should not be considered a ‘road map’ of your skin’s future.
Is There A Rosacea Cure?
Rosacea is a chronic skin condition, which means there is no cure. It does have periods of remission and relapse and can improve with treatment and management. It’s a multifactorial condition that requires a multifactorial approach to treatment, which will differ from person to person which is why there is no ‘one-and-done’ treatment plan.
Tough love time: Anyone claiming that they have a ‘rosacea cure’, that they ‘reversed’ their rosacea, or that they have ‘the secret doctors don’t want you to know’ is a grifter who cares more about their bank balance than your health and safety. Please do not be taken in by this.
Rosacea is a progressive condition, so it will get worse over time if untreated. But there are lots of things you can do to help your skin. The fact there is no cure does not mean there is no help.
This is why it’s so important to be diagnosed by a healthcare provider (HCP) and begin to regain control of your skin. As your skin becomes more stressed and prone to flare ups, the capillaries weaken, which means they are more visible, which then results in permanent redness. This is why I always recommend going to see your HCP, even if you don’t think your skin is ‘bad enough’.
Changes To The Rosacea Classifications
As I mentioned earlier, we have had numbered rosacea classifications for decades. Often rosacea sufferers will refer to themselves as type 1 or type 2, using this as a catch-all description that sums up their symptoms. However, sufferers and doctors alike have found that these neat little boxes with labels are often hard to diagnose. Which is why healthcare professionals are moving more towards phenotypes when it comes to rosacea diagnosis.
It is not uncommon for a single patient to have signs and symptoms of more than one subtype of rosacea; some patients will progress from one subtype to another (as I did); and we all have very different symptoms (e.g. my experience of rosacea type 2 may present very differently to someone else’s).
So, as per this article on Rosacea.org, medical practitioners are now encouraged to use the new rosacea classifications to discuss or classify rosacea in phenotypes (which sounds complicated but basically just means the many different characteristics common to those of us with rosacea). This new approach aims to be a more patient-centric and individual approach to diagnosis and treatment. Overall the Rosacea.org website is a great resource, but the articles can be a little dense and hard to digest, so I’ve tried to break down the key points below.
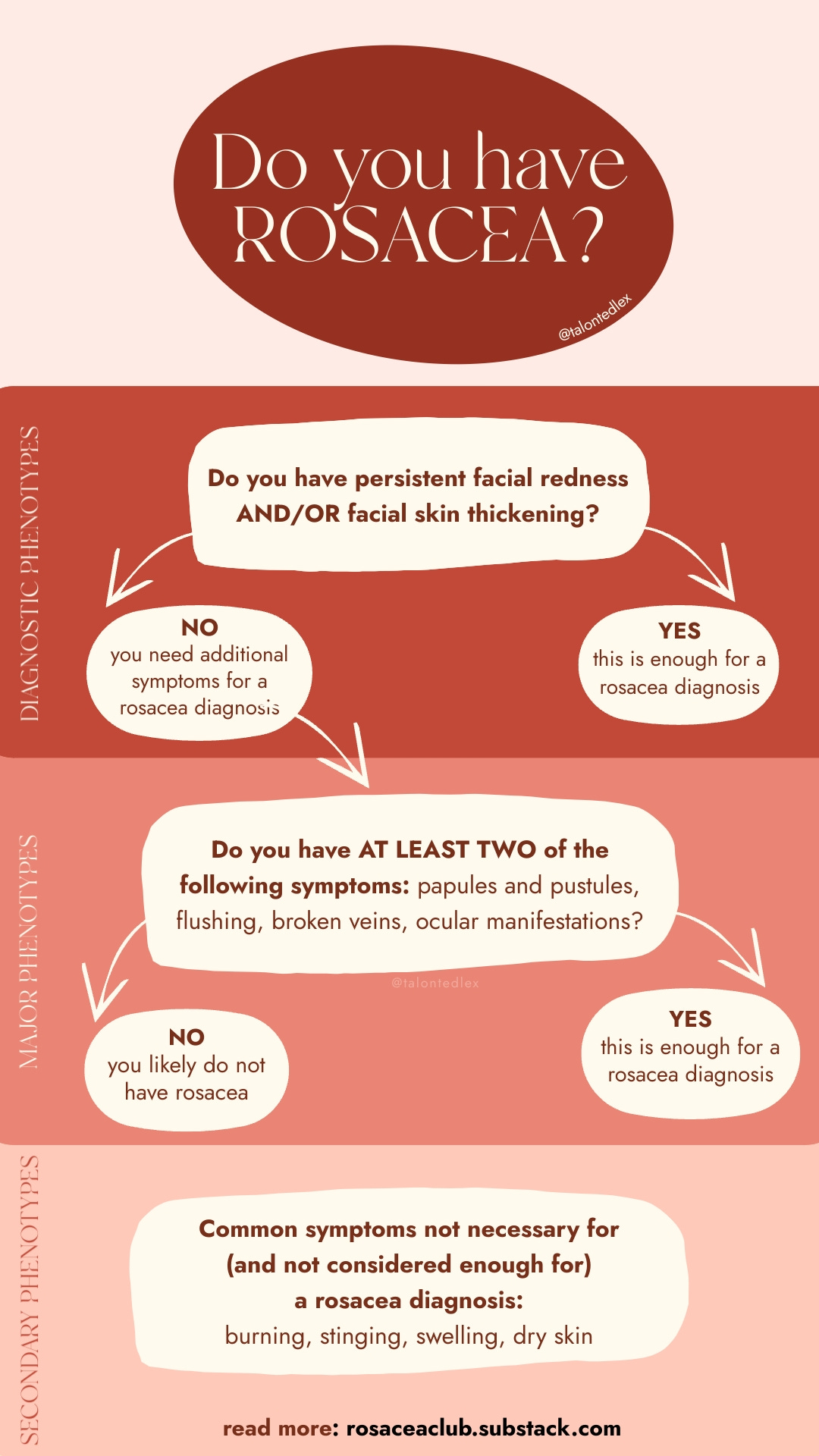
I’m going to start with a visual because that’s how I absorb information better, and maybe you’re the same. This flow chart shows how these phenotypes work in practice:
So let’s dig into the details of this chart.
Because rosacea presents as a consistent inflammatory condition across all sufferers, it’s thought that breaking the symptoms down into more specific individual phenotypes would be more useful.
These phenotypes are split into DIAGNOSTIC, MAJOR and SECONDARY:
DIAGNOSTIC PHENOTYPES
To put it simply, if you present with either persistent facial redness or facial skin thickening, that is now enough to get a rosacea diagnosis.
MAJOR PHENOTYPES
Major phenotypes are symptoms that often appear alongside the above diagnostic phenotypes. If you don’t have either of the diagnostic phenotypes (persistent facial redness or facial skin thickening), you can still be diagnosed with rosacea if you have at least two of the major phenotypes: papules and pustules, flushing, telangiectasia (broken veins) and certain ocular manifestations.
SECONDARY PHENOTYPES
Secondary phenotypes are symptoms that aren’t ‘must-haves’ for diagnosis and are not considered enough to form a diagnosis by themselves. These are: burning or stinging, swelling (oedema) and dry appearance. They might show up as part of your rosacea, but their existence alone wouldn’t indicate rosacea to a professional.
By splitting these phenotypes out, medical practitioners will be able to tailor a patient’s diagnosis, treatment, and classification with more care. They will give a more standardised criteria for research, analysing results, comparing data across rosaceans as a whole, as well as giving a more specific diagnosis to individual sufferers.
I think, on a patient level, the original subtypes will continue to be used as it’s really hard to completely phase out terms that have been used and understood for 23 years. But I wanted to explain these changes to prepare you, in case your doctor refers to phenotypes in an appointment. I think it’s fascinating to see the new ways in which rosacea is being understood and categorised – it’s definitely a step in the right direction. It’s also a good way to track the changes in your skin, as phenotypes can be added and removed from your diagnosis as time goes on.
In order for the new rosacea classifications of phenotypes to make it into common language used by patients, I think there might need to be some simplifying of the terminology: it’s easy for me to classify my rosacea to another sufferer by saying ‘type 1 or type 2’, whereas no one is going to say ‘I have rosacea, let me list my 7 individual phenotypes…’!
I wonder if a coding system would be more user friendly, with each phenotype having a letter or number representative. E.g. ‘I have rosacea: phenotypes D1-M234-S123’ or something similar. Obviously that’s still a lot more complicated than ‘type 2’ but would definitely be more useful.
What do you think? Are you in the ‘if it’s not broke don’t fix it’ camp, or do you think this will help to improve diagnosis and treatment? Let me know in the comments below!
I hope you found this blog post helpful or at least found it as interesting as I did! If you want to read the details of the article for yourself, this is the link.